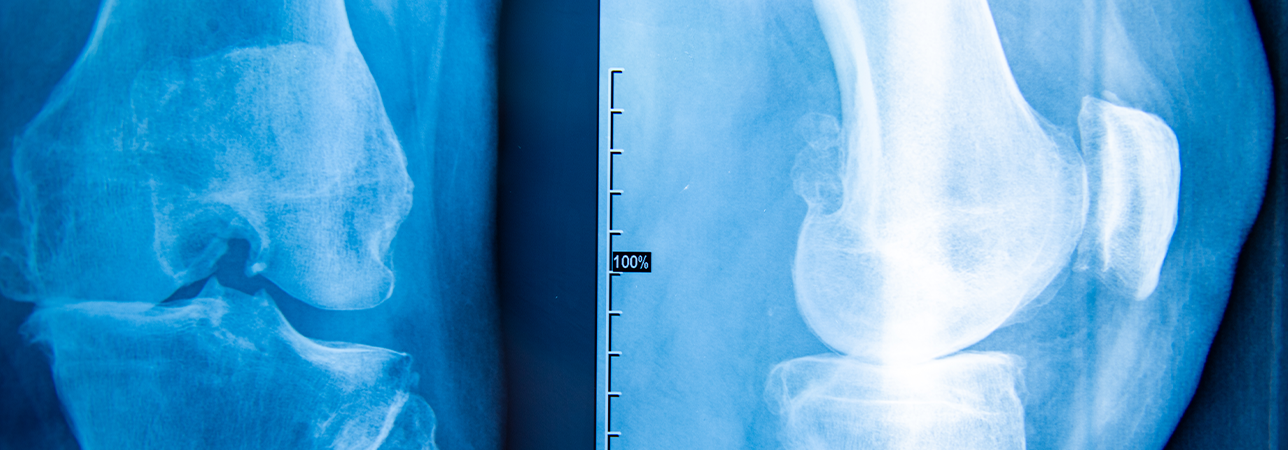
- Start-up pain and pain with certain types of exertion.
- Even minor cartilage damage can cause severe exertion-induced pain.
- There is also inflammation and swelling in the knee.
- Patients report that the knee feels unstable, they are unsteady when walking and the knee buckles when walking.
- If the condition is left untreated, even minor cartilage damage can trigger osteoarthritis.
-
Centres
back
Centres
- Specialities
- Doctors
-
Patients & visitors
- About us
- Referring doctors
- Centres
- Specialities
- Doctors
-
Patients & visitors
back
Patients & visitors
- About us
- Referring doctors
close search