Fibroids
Benign diseases of the uterus or diseases in which the uterus is affected are often very complicated.
In addition to endometriosis, these uterine diseases include severe, painful and irregular menstrual bleeding, cysts, polyps, fibroids, dropping of the uterus or inflammation of the uterus.
All these diseases can lead to significant limitations in the quality of life of the patient. Fortunately, they can be treated successfully in most cases.
Uterine diseases
The uterus is a hollow organ, whose shape resembles an upside-down pear. The baby grows up inside the uterus during pregnancy. As such, the uterus is susceptible to a variety of diseases, with endometriosis among the most common uterine diseases. Other possible conditions include:
- Fibroids, i.e. benign muscle growths in the uterus. Uterine fibroids are the most common benign tumours in women. They are not dangerous in themselves, but sometimes cause discomfort and can lead to serious complications.
- Cysts are cavities in which fluid accumulates. They can sometimes be reduced in size by taking medication. Uterine cysts usually cause patients problems if they have grown considerably or burst and have caused bleeding. Cysts can be removed surgically, which is usually performed laparoscopically.
- Polyps are growths in the uterine mucosa and occur mainly during menopause. They are removed as part of a uterine endoscopy or scraping.
- The pelvic floor muscles support the uterus. If these muscles are too weak, the uterus protrudes into the vagina. As a result, adjacent organs such as the bladder, urethra and rectum usually move from their original position. Mild symptoms of this dropping can often be corrected with the appropriate pelvic floor training; however, if the symptoms and dropping worsen, usually only surgery can help to restore the normal position of the internal organs.
- Infection of the uterus is almost always preceded by infection of the vagina. As a rule, uterine infection is treated by administering an antibiotic. If drug treatment is unsuccessful, the infected sites can be removed in a minor operation. In the case of severe infection, removal of the uterus may be necessary.
Symptoms
Most fibroids are small, not noticeable and are discovered by chance during a routine check by a gynaecologist. This means that many women do not even feel that they have fibroids; some women only have one fibroid and others have several. Fibroids are most commonly associated with symptoms in women between the ages of 30 and 50. The most common symptoms include:
- Severe or prolonged menstrual bleeding
- Bleeding between periods
- Severe, spasmodic period pain
- Pain and feelings of pressure in the abdomen requiring clarification
- Pressure and the feeling of having foreign body in the lower abdomen
- A swollen abdomen (in the case of large fibroids)
- Strong urge to urinate (if the fibroid is pressing on the bladder, which sits next to the uterus)
- Pain during sexual intercourse
- Pressure on other organs, which may lead to damage to the bladder, kidneys and rectum in the form of cystitis, constipation or back pain
- Fatigue and loss of stamina due to anaemia
In most patients, the above-mentioned symptoms mainly occur in the time before and during their monthly period. However, in the case of pronounced fibroids, the symptoms may persist over a longer period of time.
Causes
Fibroids are stimulated by female sex hormones (i.e. oestrogen and progesterone). Under the influence of hormones, the growths begin to grow. Conversely, this means that fibroids cannot grow without the hormones produced by the woman’s body. Therefore, fibroids only appear after puberty.
After the last period, i.e. the menopause, fibroids normally no longer continue to grow as the hormone levels drop again.
Furthermore, hereditary factors also likely play a role in the development of fibroids. Fibroids are more common in women whose mothers also suffer(ed) from fibroids. It is also observed that women with severe obesity develop fibroids more frequently, although it is not clear whether the obesity itself contributes to the formation of fibroids.
Fibroids, on the other hand, are rarer in women who have given birth several times and in women who have been taking the contraceptive pill for several years.
Diagnosis
Fibroids are diagnosed by a specialist as part of a gynaecological examination. This includes palpation in which larger fibroids are often already discovered. An ultrasound examination can also provide information – especially if the fibroids are smaller and thus difficult to palpate. This is usually done via the vagina. In isolated cases, an MRI scan (magnetic resonance imaging) is ordered to determine the exact extent and location of the fibroids and their relationship to the surrounding organs.
In addition, an examination of the uterus (hysteroscopy) may be necessary (in the case of fibroids that have settled on the inside of the uterus). If, on the other hand, the fibroids are located on the outside of the uterus, a laparoscopy may be the method of choice.
If the fibroids press on the urinary tract, the gynaecologist may perform a kidney ultrasound, possibly in conjunction with a pyelogram. A pyelogram is the imaging of the urinary tract with the aid of a contrast agent under X-ray radiation.
Last but not least, the doctor can arrange for a blood test and analysis of the patient’s hormone levels.
Treatments
Fibroids are only treated if they cause pain, impair fertility and thus the desire to have children, or could lead to problems during pregnancy. Therefore, when choosing a suitable therapy method, it is important to consider whether or not a woman is still trying to conceive. Which therapies are considered also depends on the severity of the symptoms and the size and location of the fibroids.
The objectives of fibroid treatment are to reduce menstrual bleeding, alleviate any pain, cramps and feelings of pressure, resolve problems associated with emptying the bladder and with digestion and maintain or optimise fertility.
Gynaecologists have several treatment options to choose from:
- Hormone treatment with a contraceptive pill to reduce the heaviness or length of menstruation or the administration of hormone preparations that inhibit the formation of oestrogen. The aim of this treatment method is to prevent the fibroids from growing and, in the best case, even shrink them as a result of the preparations used.
- Surgery to remove the fibroids or the entire uterus (hysterectomy) via the vagina, an abdominal incision or a laparoscopy.
- Removal of the (minor) fibroids (enucleation) in patients who wish to conceive in future. The doctor tries to remove the fibroid in isolation using an abdominal incision or through the vagina. Laparoscopic removal is also possible whereby three small incisions are made in the abdominal wall before the surgeon cuts out the fibroid using a long, narrow tube – the laparoscope.
- Occlusion of the blood vessels that supply the fibroids (known as percutaneous transcatheter embolisation) with the aim of causing the fibroids to shrink.
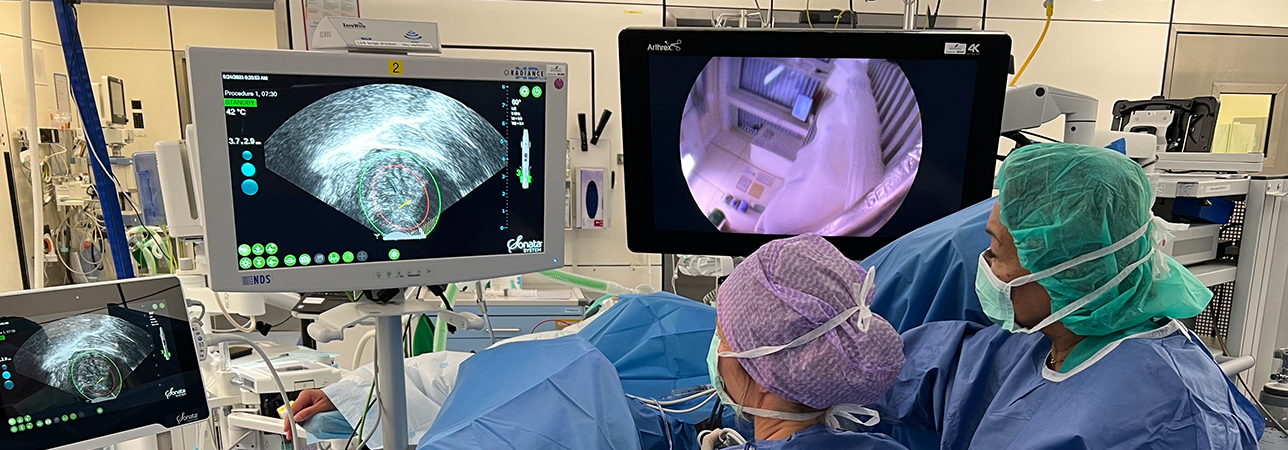
- A focused ultrasound: the fibroid is heated by very strong ultrasound waves and destroyed. The patient lies on her stomach above a sound source that emits high-frequency sound waves that are directed precisely at the fibroid.
- Drug treatment, for example, with painkillers.
-
Radiofrequency ablation is a minimally invasive surgical method that makes it possible to treat fibroids without incisions and with little pain and gently due to using heat. The heat treatment shrinks the fibroids within weeks and months.
Aftercare
Painkillers are to be taken after consultation with the gynaecologist, who will also carefully monitor the efficacy of hormonal treatment.
As the above-mentioned surgical methods do not cause extensive injuries, no special behaviour is usually required in this regard. However, patients are usually advised to take it easy for a while and to refrain from heavy physical work and intensive exercise for the first four weeks after the operation.
In general, regular gynaecological check-ups are recommended for patients with suspected fibroids or who have already been diagnosed with one or more fibroids.
FAQs
What kinds of fibroids are there?
Fibroids are benign tumours that develop from muscle cells. Depending on the type of muscle cell affected, fibroids are differentiated into the following types:
- A leiomyoma develops from smooth muscle cells and settles on the internal organs (womb, kidneys, gastrointestinal tract)
- A rhabdomyoma develops from the striated muscles, which are located on the skeletal muscles and the heart.
- Fibroleiomyoma – in this case, the growth also develops from smooth muscle cells, but also contains parts of the connective tissue.
How are fibroids differentiated?
Fibroids consist of muscle cells and connective tissue and vary according to size, shape and location. They are differentiated according to the place where they have settled in the uterus:
- Submucosal fibroids are located directly under the uterine mucosa
- Intramural fibroids are located in the uterine wall
- Subserosal fibroids are located on the outside of the uterus
- Cervical fibroids are attached to the cervix
- Intraligamentary fibroids are located in the connective tissue on the side of the uterus
Can fibroids degenerate and become a malignant tumour?
No – today’s experts believe that a fibroid does not develop into a malignant tumour (known as a sarcoma), but rather that a sarcoma develops independently of a fibroid. In contrast to benign fibroids, the sarcoma penetrates the surrounding tissue. Furthermore, cancer cells can reach more distant tissue via the blood and lymph vessels and form metastases there. Treatment of a sarcoma depends on its stage at the time of discovery and differs clearly from therapy for a fibroid.
Do fibroids affect pregnancy?
Yes, fibroids can cause problems during pregnancy. Due to the severely altered female hormone levels during pregnancy, fibroids can increase considerably in size during this time and significantly increase the woman’s risk of miscarriage or premature birth. In addition, fibroids can complicate the development of pregnancy as they prevent the embryo from being implanted into the uterine cavity. In individual cases, the gynaecologist decides whether a fibroid needs to be treated in a woman trying to conceive or in a pregnant woman, and if so, in what form.


