Surgical procedure
With surgical treatment, an operation is carried out to remove the diseased femoral head and parts of the femoral neck.
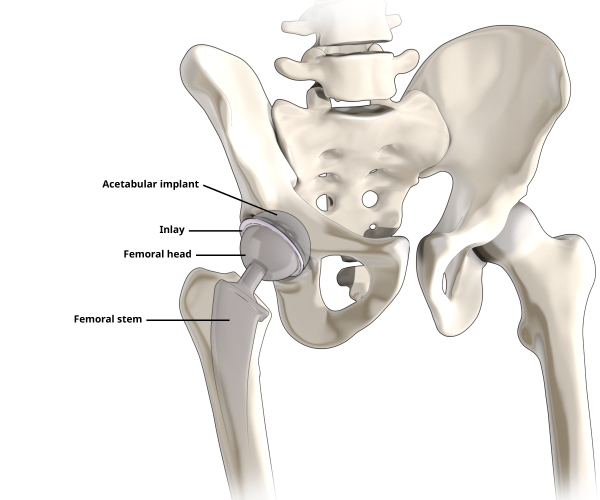
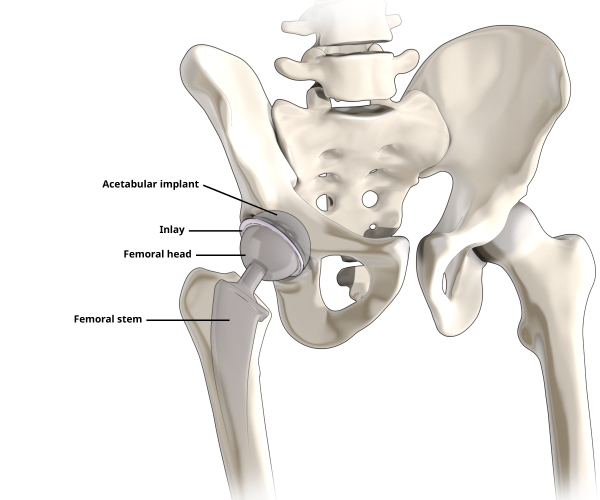
The natural hip socket is then prepared so that a new artificial hip socket can be anchored to it. The prosthetic head is then attached to an artificial shaft and the artificial hip joint is constructed.
Thanks to the advanced method of keyhole surgery, which helps to preserve the tissue, the stabilising hip muscles are only pushed to the side, rather than being severed as they were before. In this minimally invasive procedure, the artificial hip joint is introduced from the front. An incision of about eight centimetres is made in the skin, through which the artificial hip joint is inserted without injuring the tissue.
The hip operation takes up to two hours and the hospital stay is around two to five days.
What happens during a hip prosthesis operation?
- Exposure of the hip joint: Minimally invasive procedure in which the affected hip joint is exposed without damaging the tissue, and the joint capsule is removed.
- Removal of the femoral head: A saw is used to separate the worn femoral head and femoral neck from the femur itself.
- Preparation and replacement of the hip socket: The surgeon begins reconstructing the hip using the new artificial hip joint. The hip socket is prepared and the old capsule and cartilage tissue are removed from the socket. Then the new hip socket and the corresponding inlay (cartilage replacement) are inserted.
- Preparation of the femur and insertion of the shaft: The hollow interior of the femur (marrow cavity) is prepared. Trial hip repositioning – the stability of the hip is tested using trial components. If stability is guaranteed, the new hip prosthesis is used. If the quality of the bone means that the it cannot be anchored without cement, then the prosthesis is cemented in place.
- Repositioning of the new artificial hip: The artificial hip joint is repositioned and the flexible connection between the shaft and socket is restored.