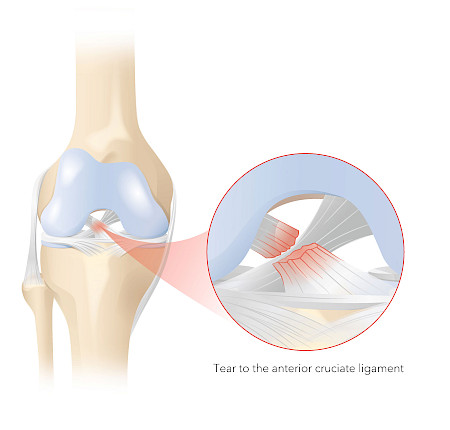
If the cruciate ligament is torn directly or near the femur, cruciate ligament reconstruction surgery can be carried out to preserve the ligament. During the procedure, the torn cruciate ligament is stabilised and reattached using a strong thread. This is followed by a cruciate ligament suture, which helps the torn ligament to heal itself.
The procedure is performed using minimally invasive arthroscopy (joint endoscopy). Concomitant injuries (e.g. a meniscus tear or cartilage damage) can be treated in the same operation.